

NODAT: Time for a paradigm shift? We may be missing the window of opportunity...
New Onset Diabetes after Transplant (NODAT) occurs in nearly a quarter of Renal Transplant Recipients (RTR) (1). Similar incidence has been reported in lung [2] , liver [3] and cardiac transplant recipients. NODAT is common and negates the benefits of transplantation in many ways. NODAT is associated with shortened graft and patient survival, increased risk of infection, and increased cardiovascular events. [4, 5]
While Post transplant hyperglycemia is very common and portends the development of NODAT [6], the ideal time frame for the diagnosis of NODAT is not settled. Many cases of NODAT will be missed if the diagnosis is based on Fasting Plasma Glucose alone, as the hyperglycaemia tends to occur post prandial. The use of HbA1c early in the post-transplant period for the diagnosis of NODAT is fraught with inaccuracies due to usually low and unstable Haemoglobin levels. OGTT captures the glycemic abnormalities including IGT more accurately [7].
The etiopathogenesis of NODAT is multifactorial. Apart from non-modifiable factors such as increased age, ethnicity and family history, there are modifiable factors such as medications, physical activity and diet post-transplant. HCV infection [8,9] has been associated with increased risk of developing NODAT. In a case series, among the 16 RTRs who had received Interferon-alpha and had cleared HCV Viremia, none developed NODAT.[10]It will be interesting to study the impact of recent success with HCV eradication treatment on NODAT in prospective trials.
Immunosuppressive medications play a major role in the causation of NODAT. Calcineurin Inhibitors (CNI) have been associated with NODAT. CNI cause pancreatic beta-cell exhaustion and decreased uptake of glucose by the muscles and adipocytes. Tacrolimus (Tac) is more potent as an immunosuppressive agent but also is a more potent diabetogenic drug compared to Cyclosporine (CyA). [11]. In a retrospective study of 54 RTR on Tac who developed NODAT, Ghisdal et al studied the effect of conversion from Tac to CyA in 34 while the remaining 20 RTR were continued on Tac. Fasting Blood Glucose and HbA1c decreased significantly at 1 year follow up in those converted to CyA with no adverse effect on graft and patient survival. [12] A prospective RCT is underway. (EudraCT no. 2006-001765-42) mTOR inhibitors have also proved to be diabetogenic. In a Meta-analysis of 7 RCTs involving 2083 RTR (mTOR inhibitors: 1179; controls: 904), conversion from CNI to mTOR inhibitors did not decrease the risk of NODAT and in fact was associated with a non significant increase in NODAT. [13]
As reported in BENEFIT and BENEFIT-EXT studies, patients on Belatacept had a lower incidence of NODAT compared to those on CyA. [14]
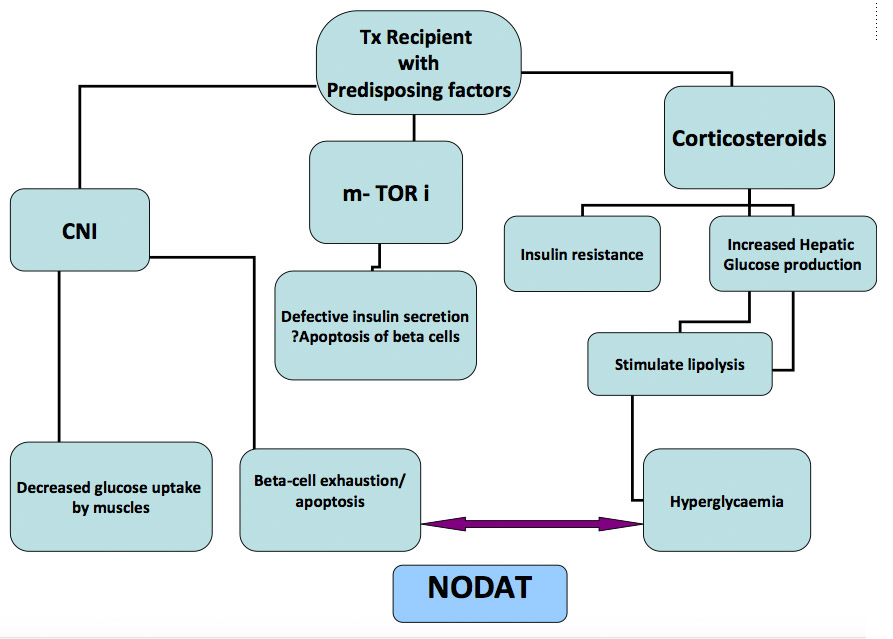
Figure 1: Immunosuppressive Medications and NODAT
Corticosteroids cause NODAT predominantly by causing peripheral insulin resistance. Previous attempts at rapid steroid withdrawal have not been very encouraging with increased incidence of acute rejection episodes.[15] In a recent landmark study, Thomusch et al compared induction with rabbit ATG and Basiliximab for rapid steroid withdrawal on Day 8, compared to steroid maintenance therapy in patients at low immunologic risk. The incidence of NODAT in the rapid steroid withdrawal arms with either Basiliximab or rabbit-ATG was 24% and 23% respectively compared to 39% with steroid maintenance therapy. (p=0·0004) There were no differences in the incidence of biopsy proven rejection or patient survival at 12 months among the three groups. [16]
Yates et al looked at the effect of twice daily divided doses of Prednisolone compared to single daily dose and reported reduced glycemic excursion and hyperglycaemia in patients on twice daily dose of Prednisolone. [17] The traditional approach has been to modify lifestyle factors, add Oral Hypoglycaemic Agents (OHA) and finally Insulin, in a stepwise fashion, similar to the approach in DM Type 2. However, nearly 50% of the pancreatic beta cells are dysfunctional by the time IGT becomes manifest. [18]Thus, by adopting the time honoured approach, we may be losing the window of opportunity to reverse the damage to the pancreatic beta cells. It is well established in experimental animals that severe hyperglycaemia itself is toxic to pancreatic beta cells.[19,20]In humans, transient hyperglycemia in the first 3 months antedates the development of NODAT in a vast majority of patients. [6] By normalizing the plasma glucose early post transplant, the pancreatic beta cells may be spared from the vicious cycle of glucotoxic injury and resultant hyperglycemia, and ultimately the development of NODAT.
Studies have looked at achieving near euglycemia and resting the pancreatic beta cells by the use of exogenous insulin in patients at risk of developing type 2 DM and in NODAT. In the Outcome Reduction with an Initial Glargine Intervention (ORIGIN) trial, there was a subgroup of 1456 participants with IGT. At randomization, 737 of those 1456 subjects were assigned to Insulin Glargine and 719 assigned to standard care. Those who were started on Insulin Glargine were 28% less likely to develop DM after 6 years of follow up. [21]
Similar beta-cell sparing with early intensive Insulin therapy was reported in post-transplant hyperglycaemia. In a proof -of-concept study, Hecking et al assigned 50 RTR who developed post transplant hyperglycaemia on Tac to Insulin therapy or standard of care therapy with oral medications. All the 25 patients who received Insulin treatment initially were insulin-independent at 12 months of follow up, while 28% of the controls required ongoing treatment with antidiabetic agents. [22] It is hoped that a larger multicentre trial which is underway will confirm the benefits of such an approach in preserving the beta-cell function and reducing the incidence of NODAT (Clinical Trials NCT 01683331).Results are expected in early 2018.
Harrison et al reported that β-Cell function can be preserved for at least 3.5 years with early and intensive therapy for 3 months consisting of Insulin and Metformin. After a 3 month lead in therapy with insulin and metformin, the subjects were assigned to either insulin plus Metformin or to triple oral therapy consisting of Metformin, Sulfonylurea and Glitazone. Both the groups showed excellent glycemic control and retained beta cell activity as measured by C-peptide throughout the study period. [23]
While exogenous insulin has sound pathophysiologic basis of resting the pancreatic beta cells in the prevention of NODAT, there are some practical difficulties in its application in the real world, with the need for patient education, titrating the dose, episodes of hypoglycaemia and weight gain. However, currently there is no evidence in the form of large randomized trials, to suggest safe and efficacious use of any particular OHA in the treatment or prevention of NODAT. [24]
Lifestyle modifications should start pre transplant in overweight/obese patients with specific aims at weight reduction and continued vigorously post-transplantation, in parallel with the other measures discussed. The Finnish Diabetes Prevention Study in 522 middle aged, overweight subjects with IGT showed a 58 % reduction in the incidence of T2DM with lifestyle intervention involving weight reduction and increased physical activity. [25]Similar benefits of intense life style intervention was reported in transplant recipients with impaired glucose tolerance or NODAT. [26]
Early and intense life style intervention in patients listed for transplant, rapid steroid withdrawal in low risk patients, dividing the daily dose of Prednisolone, and changing from Tac to CyA when appropriate, could minimize the risk and impact of NODAT. Perhaps a very important step will be the early institution of Insulin to rest the pancreatic beta cells. The transplant community has to brace itself to the changing paradigms in the prevention and management of NODAT.
References:
- Kasiske BL, Snyder JJ, Gilbertson D et al.
Diabetes mellitus after kidney transplantation in the United States
Am J Transplant. 2003; 3(2):178–185 - Hackman KL, Snell G, Bach LA.
Prevalence and predictors of diabetes after lung transplantation: a prospective, longitudinal study.
Diabetes Care. 2014; 37(11):2919-25. - Baid S, Cosimi AB, Farrell ML, et al.
Posttransplant diabetes mellitus in liver transplant recipients: risk factors, temporal relationship with hepatitis C virus allograft hepatitis, and impact on mortality
Transplantation.2001;72: 1066–107 - Cosio FG, Hickson LJ, Griffin MD et al
Patient Survival and Cardiovascular Risk After Kidney Transplantation: The Challenge of Diabetes.
Am J Transplant. 2008; 8(3):593-9 - Hjelmesaeth J, Hartmann A, Leivestad T, et al.
The impact of early-diagnosed new-onset post-transplantation diabetes mellitus on survival and major cardiac events
Kidney Int 2006; 69: 588–595 - Chakkera H A, Knowler W C, Devarapalli Y et al
Relationship between Inpatient Hyperglycemia and Insulin Treatment after Kidney Transplantation and Future New Onset Diabetes Mellitus
Clin J Am Soc Nephrol. 2010 Sep; 5(9): 1669–1675 - Sharif A, Moore RH, Baboolal K.
The use of oral glucose tolerance tests to risk stratify for new-onset diabetes after transplantation: an under diagnosed phenomenon.
Transplantation. 2006; 82 (12):1667–1672 - Bigam D, Pennington J, Carpentier A, et al.
Hepatitis-C related cirrhosis: a predictor of diabetes after orthotopic liver transplantation.
Hepatology.2000; 32 (1):87–90. - Shah T, Kasravi A, Huang E, et al.
Risk factors for development of new-onset diabetes mellitus after kidney transplantation.
Transplantation 2006; 82: 1673–1676 - Kamar N, Toupance O, Buchler M et al
Evidence that Clearance of Hepatitis C Virus RNA after α-Interferon Therapy in Dialysis Patients Is Sustained after Renal Transplantation
J Am Soc Nephrol, 2003: 14: 2092-2098 - Vincenti F, Friman S, Scheuermann E et al. .
Results of an international, randomized trial comparing glucose metabolism disorders and outcome with cyclosporine versus tacrolimus,
Am J Transplant 2007; 7: 1506-1514 - Ghisdal L, Bouchta NB, Broeders N et al
Conversion from tacrolimus to cyclosporine A for new-onset diabetes after transplantation: a single-centre experience in renal transplanted patients and review of the literature
Transplantation International 2008; 21 (2): 146–151 - Murakami N, Riella LV, Funakoshi T
Risk of Metabolic Complications in Kidney Transplantation After Conversion to mTOR Inhibitor: A Systematic Review and Meta-Analysis
Am J Transplantation 2014; 14: 2317–2327 - Vanrenterghem Y, Bresnahan B, Campistol J, et al.
Belatacept-based regimens are associated with improved cardiovascular and metabolic risk factors compared with cyclosporine in kidney transplant recipients (BENEFIT and BENEFIT-EXT studies).
Transplantation 2011; 91: 976–98314. Steroid Avoidance or Withdrawal for Kidney Transplant Recipients - Pascual J, Zamora J, Galeano C et al.
Cochrane Database Syst Rev. 2009; (1):CD005632. - Thomusch O, Wiesener M, Opgenoorth M, et al
Rabbit-ATG or basiliximab induction for rapid steroid withdrawal after renal transplantation (Harmony): an open-label, multicentre, randomised controlled trial
Lancet 2016; 388: 3006-3016 - Yates CJ, Fourlanos S, Colman PG et al
Divided dosing reduces prednisolone-induced hyperglycaemia and glycaemic variability: a randomized trial after kidney transplantation
Nephrol Dial Transplant (2014) 29: 698–705 - Abdul-Ghani MA, Tripathy D, DeFronzo RA.
Contributions of beta-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose.
Diabetes Care. 2006; 29:1130–9.16 - Zhang TZ, Li J, Yang L et al
Cytotoxic Role of Intermittent High Glucose on Apoptosis and Cell Viability in Pancreatic Beta Cells
Journal of Diabetes Research Volume 2014 (2014), Article ID 712781, 9 pages - Leahy JL, Bonner-Weir S, Weir GC
Beta-cell dysfunction induced by chronic hyperglycemia. Current ideas on mechanism of impaired glucose-induced insulin secretion.
Diabetes Care 1992 15(3): 442-455 - The ORIGIN Trial Investigators
Basal Insulin and Cardiovascular and Other Outcomes in Dysglycemia
N Engl J Med 2012; 367:319-328 - Hecking M,* Haidinger M,* Döller D, et al
Early Basal Insulin Therapy Decreases New-Onset Diabetes after Renal Transplantation
J Am Soc Nephrol, 2012; 23(4): 739–749. - Harrison LB, Adams-Huet B, Raskin,P et al
β-Cell Function Preservation After 3.5 Years of Intensive Diabetes Therapy
Diabetes Care. 2012 Jul; 35(7): 1406–1412. - Sharif A, Hecking M, de Vries APJ et al
Proceedings From an International Consensus Meeting on Post transplantation Diabetes Mellitus: Recommendations and Future Directions
Am J Transplantation 2014; 14: 1992–2000 - Tuomilehto J, Lindstrom J, Eriksson JG, et al.
Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance.
N Engl J Med. 2001; 344:1343–50 - Sharif A, Moore R, Baboolal K
Influence of lifestyle modification in renal transplant recipients with postprandial hyperglycemia
Transplantation 2008; 85(3):353-8
ABOUT OUR GUEST EDITOR
 Jagadish S. Jamboti
Jagadish S. Jamboti
Consultant Renal Physician, Fiona Stanley Hospital
Murdoch, Western Australia
Senior Clinical Lecturer at the University of Western Australia
Adjunct Senior Lecturer at the Notre Dame University at Fremantle
Dr Jagadish S Jamboti trained to be a Nephrologist in Mumbai, India in 1995 and migrated to Australia in 2000. He trained at Westmead Hospital, Sydney, Princess Alexandra hospital, Brisbane and at Royal Perth Hospital, Perth. Australia. He is currently a Consultant Renal Physician at Fiona Stanley Hospital, Murdoch, Western Australia and a Senior Clinical Lecturer at the University of Western Australia and Adjunct Senior Lecturer at the Notre Dame University at Fremantle. He is especially interested in Viral infections post renal-transplant and Cardio-renal syndromes. He was appointed as an Educational Ambassador by the International Society of Nephrology in 2015 and is keen to share his passion for providing quality and affordable renal care in developing countries.
Webinar for YOUR Fellows and Students
OPEN TO MEMBERS AND NON-MEMBERS.
FORWARD THIS EMAIL TO YOUR FELLOWS!
|
|
THURSDAY, May 11, 2017, 11AM (MONTREAL TIME)Balancing Career and Personal Life: Establishing Priorities and Achieving Job SatisfactionMartha Pavlakis, MD |
Upcoming Meeting Deadlines
ISVCA 2017 - MAY 7
ABSTRACT SUBMISSION DEADLINE EXTENDED
13TH CONGRESS OF THE INTERNATIONAL SOCIETY OF VASCULARIZED COMPOSITE ALLOTRANSPLANTATION (WWW.ISVCA2017.ORG)
SALZBURG | AUSTRIA, OCTOBER 26 - 27, 2017
CST/CTRMS 2017 - May 8
ABSTRACT SUBMISSION DEADLINE
Joint Scientific Meeting - Canadian Society for Transplantation and Cell Transplant and regenerative medicine society (HTTP://WWW.CST-TRANSPLANT.CA/2017_CST-CTRMS.HTML) - Halifax | Canada, Sept 26-29, 2017
IPTA 2017 - May 14
STANDARD REGISTRATION DEADLINE
International Pediatric Transplant Association (http://ipta2017.org) - Barcelona | Spain | May 27-30, 2017
TSS 2017 - May 15
STANDARD REGISTRATION DEADLINE
TTS Transplantation Science Symposium (www.tss2017.org) - Victoria, BC| Canada ,May 24-26, 2017
IPTA Congress - PROGRAM NOW ONLINE
9th Congress of the International Pediatric Transplant Association
BARCELONA, SPAINMay 27 to 30, 2017
The full program for the Congress is now available for viewing through our online WebAPP (http://guide.ipta2017.org).
THERE IS STILL TIME TO REGISTER TO THE CONGRESS! CLICK BELOW FOR CONGRESS DETAILS!
Survey
Banff Highly Sensitized Working Group
As you know, a major unmet need in kidney transplantation is an effective treatment for antibody mediated rejection. To advance this field and develop effective treatment, it is important to have consistent definitions and interpretation of renal allograft histopathology findings with the eventual goal of optimizing the management of renal allograft recipient. To ultimately develop a consensus for clinical diagnosis and therapeutic interventions, we believe that it is extremely important to understand how the interpretation and management currently differ among physicians for the same clinical scenario.
This survey is designed to understand the current practice patterns for the management of antibody mediated injury of the renal allograft. Please answer the following questions based upon your current practice patterns. We want to emphasize that there are no right or wrong answers for these cases.
Please use the link below to complete the survey.
Click here to take the survey
Young Members Corner
Pursuing an academic career in transplantation: lessons from the field
Jose F Camargo, MD
University of Miami Miller School of Medicine
Young Members’ Committee of The Transplantation Society
These are very tough days for young physicians trying to pursue a career in academic medicine. Lack of funding, infrastructure and mentorship are common obstacles that halt even the most enthusiastic minds. One of the goals of the Young Members’ Committee is to engage trainees and junior faculty into research activities and facilitate continuous advancements in the field of transplantation. With hopes of providing advice to young transplanters out there, here I share some lessons learned from my research experience as junior faculty.
Lesson #1: find your niche. It is easy to get lost in numerous projects you might want to pursue. You must not only identify gaps in knowledge, but also make sure to work on something that addresses unmet needs in your local patient population and is relevant to your practice. Before starting in my current position, I did some work in pathogenesis of fungal infections. However, it did not take long for me to realize that this was not going to be an area I could continue to pursue in my new job. Instead, I noticed my current institution performs large volume of kidney transplants (>300/year) and we have one of the highest incidence of newly diagnosed cases of HIV/AIDS (52 per 100,000 residents in 2015) in the US. Thus, I focused my research efforts in studying kidney transplantation and HIV.
Lesson #2: find a mentor. Mentors can provide great advice and put your career on the fast track to success. Try to find mentors with experience of your field of interest. The Young Members’ Committee is chaired by two of the world leading experts in HIV and transplantation. Dr. Jayme Locke leaded large cohort studies that have shaped our understanding long-term outcomes among HIV+ kidney transplant recipients. Dr. Elmi Muller pioneered the HIV-positive-to-HIV-positive transplantation studies which became the basis for the HOPE (HIV Organ Policy Equity) Act signed by President Barak Obama in November 2013; initially as part of a research protocol, the HOPE act lifts the ban of using organs from HIV+ donors and is expected to dramatically shorten waiting times and increase access to kidney transplantation among HIV+ candidates. Networking is critical to find mentors and collaborators in your field so try your best to attend scientific meetings. In 2018, the 27th International Congress of The Transplantation Society will be held in Madrid, Spain, June 30 to July 5. Mark your calendar!
Lesson #3: watch for “low hanging fruit”. Getting financial support for research can be extremely difficult for young investigators. However, make sure to watch for local RFAs (request for applications) and apply to intra-mural pilot grants where your chances of getting funded are significantly higher. During my first year as junior faculty, I applied for a pilot award of the Centers for AIDS Research (CFAR), and I was funded in my first attempt! This bought me 10% of my salary effort which does not seem much but it has really helped me pursuing research projects in this area. So far, we have made important observations in the field of HIV and transplantation: i) pre-transplant CD4 count predicts depth and duration of lymphopenia and risk of infection in kidney transplant recipients who receive induction with anti-thymocyte globulin (Am J Transplant 2016;16:2463-72); ii) pathological immune activation associated with chronic HIV infection does not seem to explain the increased susceptibility to allograft rejection in this population (Transpl Immunol 2016;38:40-3); and iii) protease inhibitor-containing anti-retroviral regimens are associated with reduced 3-year graft and patient survival and increased risk of infection (F1000Res 2016;5:2893). We have also made efforts to increase awareness of complex drug-drug interactions among transplant providers (Ann Pharmacother 2017). Currently, we are studying the role of immune activation, inflammatory and microbial translocation biomarkers in the pathogenesis of acute rejection in HIV+ kidney transplants and results are expected this fall.
Lesson #4 (and most important): never give up! In the same way that I got lucky with the pilot award application, I have had many grant and article submissions rejected. The good thing, is that you usually get insightful feedback from reviewers that you can incorporate into your revised submissions. Remember many individuals worldwide will sooner or later benefit from your scientific contributions! So keep trying and never lose enthusiasm in the pursuit of academic and clinical excellence in transplantation.
If you’re interested in pursuing an academic career in transplantation and what additional advice, get in touch with us via chelsea.patriquin@tts.org.
IN THE NEWS
More Surgeons Must Start Doing Basic Science
April 22 – Nature - They say they don't have the time or incentives to do research — and that’s dangerous for translational medicine.
Read More
Transplant Ethics for the 21st Century
April 13 – BioEdge - Transplant surgery has developed rapidly since the first successful heart transplants in the late 1960s. Newly developed techniques includes uterus, penis and larynx transplantations, and some researchers may shortly attempt to transplant testicle, ovary and fallopian tubes.
Read More
Babies Floating in Fluid-Filled Bags
A lab has successfully gestated premature lambs in artificial wombs. Are humans next?
Read More
Testing Urine for Particular Proteins could be Key to Preventing Kidney Transplant Failure
April 23 – Medical Xpress - Testing for molecular markers in the urine of kidney transplant patients could reveal whether the transplant is failing and why, according to research presented at the 27th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID)
Read More
Organ Donation—A New Frontier for AI?
April 24 – Phys Org- Organ transplants are a game of odds. Success depends on a number of factors: how old and how healthy the donor is, how old and how healthy the recipient is, how good a biological match can be found, how ready the patient is to receive it. But if the system could be gamed by better statistics, would the success rate rise?
Read More
Meeting an Organ Trafficker Who Preys on Syrian Refugees
April 25 - BBC News - There's a glint of pride in Abu Jaafar's eyes as he explains what he does for a living.
Read More
Cancer Risk Rises after Childhood Organ Transplant: Study
April 26 – Medical XPress - Children given an organ transplant have a substantially higher risk of developing cancer—in some cases up to 200 times higher—than the general population, a new study finds.
Read More
Age is just a number for Stem Cell Transplant
April 22 – ET Healthworld- In terms of relapse and recovery rate there was much scope of improvement for elders diagnosed with acute Leukemia and MDS using stem cell transplants over conventional therapies.
Read More
Uterus Transplant Risky, Raises Ethical Debate
April 22 – The Times of India - In exactly three weeks, womb transplant will be a reality in India. A Pune hospital is all set to carry out the country's first set of uterine transplants, fitting three women with the wombs of their mothers.
Read More
Manipulating Select T-cells May Prevent Dangerous Side Effect of Stem Cell Therapy
April 21 – Lymphoma News Today - Controlling the balance of two subsets of immune T-cells, known as CD4+ and CD8+, after stem cell transplants makes it possible to prevent graft-versus-host disease (GVHD) while keeping the anti-cancer activity of the healthy transplanted cells, results from a preclinical study show.
Read More
Snapshots of Life: Neurons in a New Light
April 21 – NIH Blog - Birds do it, bees do it, and even educated fleas do it. No, not fall in love, as the late Ella Fitzgerald so famously sang. Birds and insects can see polarized light—that is, light waves transmitted in a single directional plane—in ways that provides them with a far more colorful and detailed view of the […]
Read More
Contact
Address
The Transplantation Society
International Headquarters
740 Notre-Dame Ouest
Suite 1245
Montréal, QC, H3C 3X6
Canada
Используйте Вавада казино для игры с бонусом — активируйте промокод и начните выигрывать уже сегодня!


